Airborne Covid Requires Them
Wearing Masks
Masks are routine protection against airborne infections in hospitals in the United States. Other countries like Japan have used them in public for to prevent illnesses as common as colds.
“I think there are cultural differences in Asia as a whole. Mask use in Korea, in Japan, Taiwan, Singapore has been relatively high throughout the pandemic. There were mandates in some parts of Asia, but even in places where there weren’t mandates, mask use was certainly higher than in other parts of the world.”
Ben Cowling, British epidemiologist at the University of Hong Kong1
Masks have been used by Asians in public for the 1918 influenza pandemic, the 2002 Severe Acute Respiratory Syndrome (SARS, the first coronavirus epidemic), and the 2012 Middle East Respiratory Syndrome (MERS, a second coronavirus).2
In the United States, there is more resistance to masks as they have become politicized:
“Mask wearing, especially being a very visible thing, becomes a part of identity, so people identify themselves partly by whether they are willing to wear masks or not.”
Donald Milton, professor at the University of Maryland’s School of Public Health3
Masking in hospitals for known patient illnesses is rigorously enforced. Patient room door signs are posted showing required isolation precautions beyond Standard or Universal (bloodborne). These extra steps might be a combination of Contact, Droplet, and Airborne precautions. Airborne N95 masks (also called respirators) are fit tested annually for hospital staff.
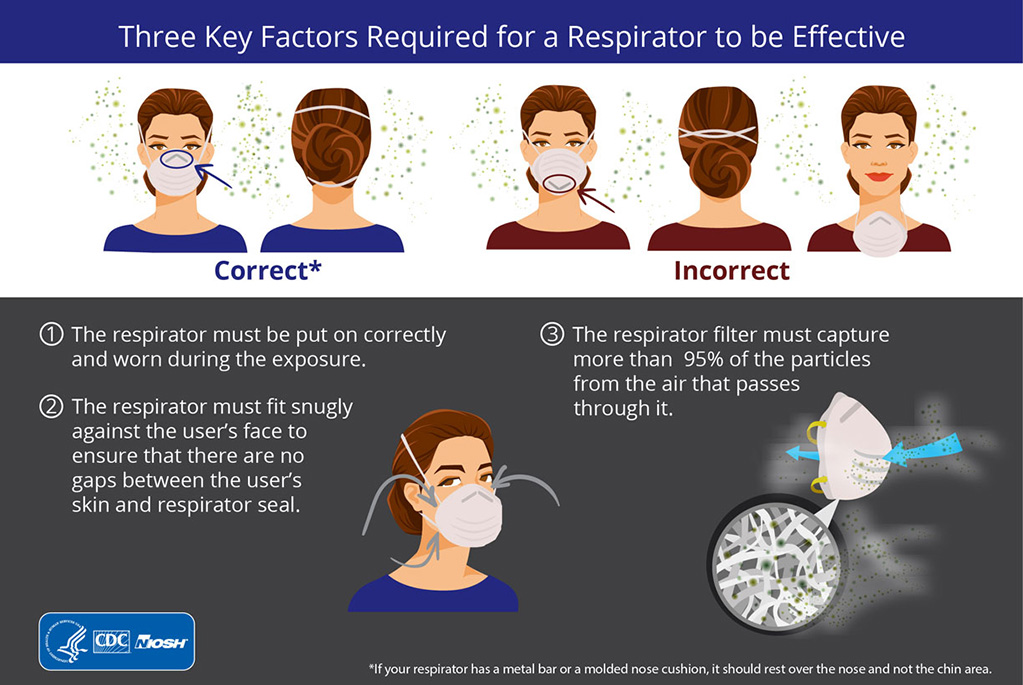
Not having the correct mask, not having it fit tested, not using it, not wearing it correctly, having a poor face seal; all these will reduce your protection. The mask for airborne precautions is a “fit-tested NIOSH-approved N95 or higher level respirator.”
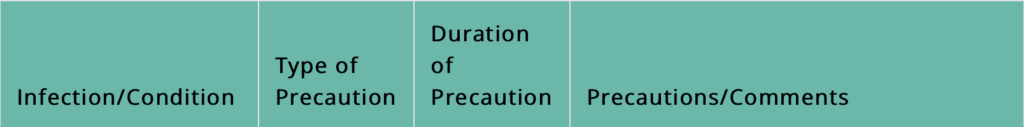
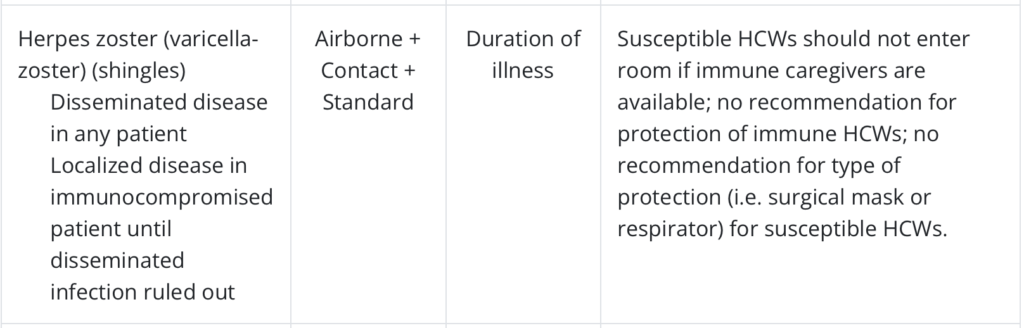
Appendix A Precautions
Every hospital in the United States has a copy of this in their infection control manual: Appendix A, “Type and Duration of Precautions Recommended for Selected Infections and Conditions” from the Centers for Disease Control and Prevention (CDC), last updated September 2018 and last reviewed July 22, 2019. It’s part of the overall “Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007).”

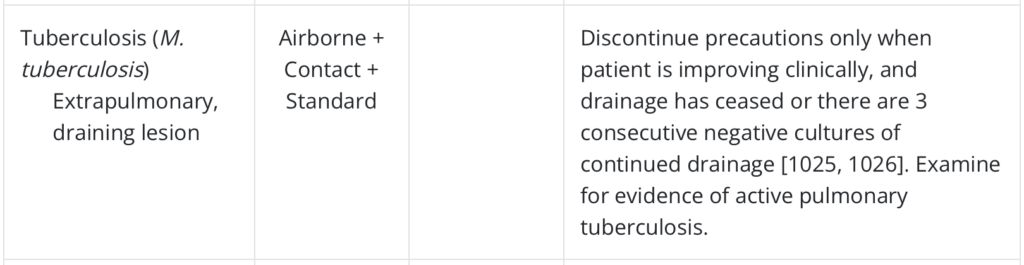
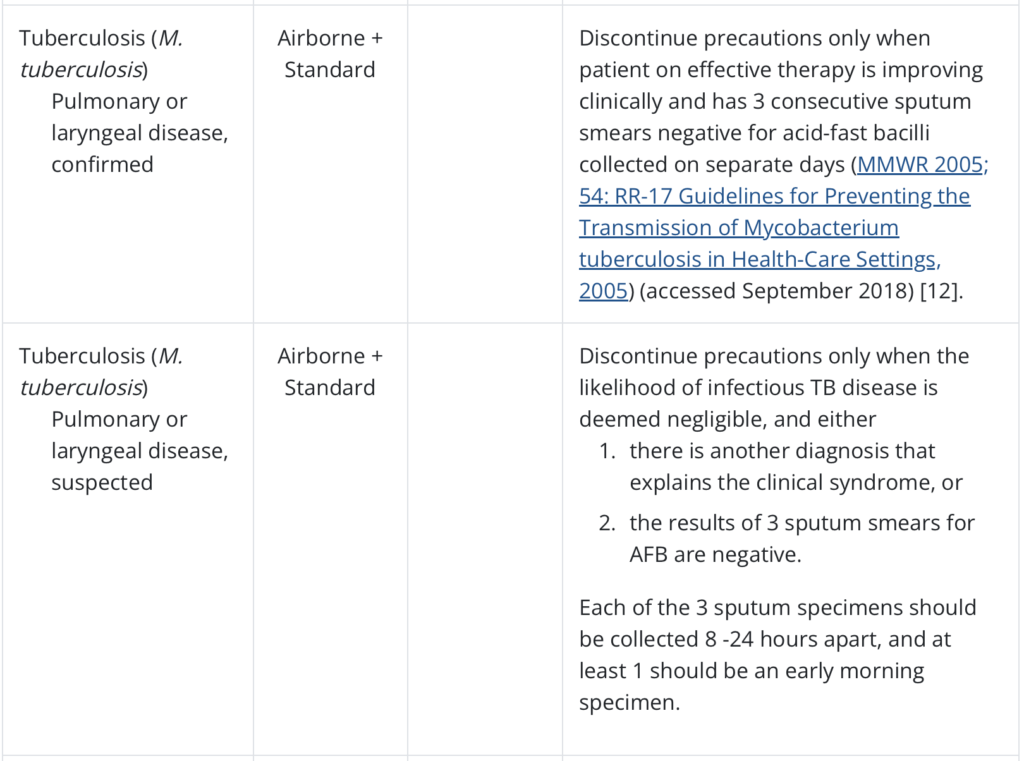

The items above include all current airborne isolation as a primary precaution; the comments section includes some conditions where airborne could be added, such as large wound drainage and irrigation.
Seven airborne entries out of 34 pages; 3 for tuberculosis, and 2 for the varicella-zoster virus: chicken pox (varicella-zoster) and shingles (herpes zoster). Appendix A has been published since 1970, for 53 years.
Covid Specifically
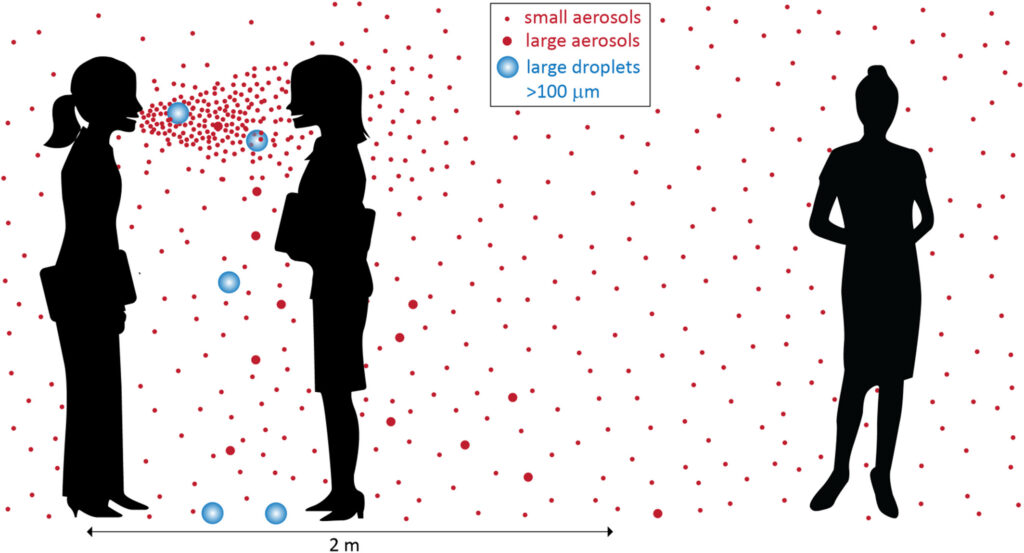
The CDC says COVID-19 (coronavirus disease-2019) is caused by the SARS-CoV-2 virus. This virus spreads on droplets and smaller particles exhaled by an infected person. The CDC Glossary calls those droplets and particles “bioaerosols,” or an “airborne dispersion of particles” that can include bacteria, viruses, or fungal spores, depending on the disease. Breathing those aerosols or contacting them with eyes, nose, or mouth can infect you.
The droplets and aerosols can also contaminate surfaces (fomites) for periods up to 3 days. This is the reason for recommendations of frequent hand washing and to avoid touching mouth, nose, or eyes.
The Appendix A entry for corona virus (SARS-CoV) directs you to SARS.
SARS-CoV-2 is genetically similar to SARS-CoV. SARS-CoV is the nearest human coronavirus relative of SARS-CoV-2 with an 86.85% similarity, which is reflected in their similar names. The currently known closest relative of SARS-CoV-2 is the bat coronavirus RaTG13 which has 96.75% similarity.
Lois Zoppi, “How does SARS-CoV-2 Compare to SARS-CoV?” News-Medical.Net, Mar 15, 2021
The isolation precautions for Covid (SARS-CoV-2) are Airborne (N95 mask) + Droplet (mask and goggles or face shield) + Contact (gloves and gown) + Standard or Universal (any equipment needed to avoid exposure to body fluids).
Note that Droplet precautions are permitted if an airborne infection isolation room (AIIR), a negative air pressure room with greater building exhaust than supply air, is not available.
Pandemic Past and Future
Proposed Masks for All Act
Senator Bernie Sanders (I-VT) has proposed the Masks for All Act since 2020 to provide every person in the United States with three free N95 masks. This was endorsed at the time by Vivek Ramaswamy as “a sensible idea,” writing that “The cost is a tiny fraction of other less compelling federal expenditures on COVID-19.” He has dropped his support, saying he no longer believes they prevent Covid and has always opposed mask mandates.5
End to Public Health Emergency
The Federal COVID-19 Public Health Emergency (PHE) ended on May 11, 2023, and the CDC and state and municipal health departments have stopped reporting Covid Community Transmission levels. The CDC admits that the reporting helped healthcare systems respond earlier, reduced patient loads, and better protected patients. So they want healthcare facilities to replace it with local “source control” by doing their own community transmission metrics and a better job of infection control at the source, including masking the patient, and possibly all healthcare providers and visitors.6
Proposed Changes to CDC Guidelines

Changes to CDC isolation guidelines7 are currently under review and receiving pushback from nurse, patient and professional groups. An advisory group, the Healthcare Infection Control Practices Advisory Committee (HICPAC), has postponed voting on them until the next meeting in November.
Opponents have said the changes are based on flawed evidence, omit key infection control tools, and uses an opaque CDC approval process with private committee votes and failure to issue draft proposals. They say the proposed guidelines weaken existing infection control standards, favoring employer and hospital costs over employee and patient safety.8 This is sometimes referred to as “the business of healthcare.” One commentator has written:
As COVID continues to cycle through new variants and surges, hospitals are stripping away even the inadequate infection control measures they implemented at the beginning of the pandemic. Come in for heart surgery, leave with a heart-damaging virus. What a business model!
Julia Doubleday, “Hospitals are killing patients because they don’t feel like doing infection control,” The Gauntlet, Aug 23, 20239
Six of nine current HICPAC voting members are affiliated with major hospitals or healthcare systems, including Ascension, Genesis Healthcare, Mass General Brigham, and Beth Israel Lahey Health.
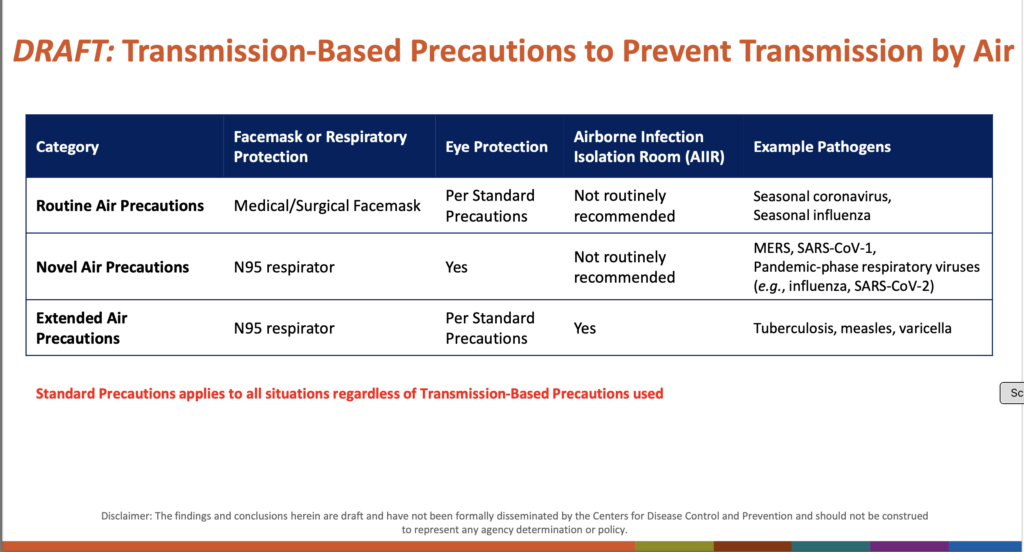
During the Covid pandemic the CDC adopted healthcare staffing policies meant to address shortages and let healthcare employers implement infection precautions based on staffing needs, including allowing healthcare personnel with active COVID to work and substituting surgical for N95 masks.10 The proposed guidelines create “Routine Air Precautions” using surgical masks for “Seasonal coronavirus” and “Novel Air Precautions” using N95 masks for “Pandemic-phase respiratory viruses” including SARS-CoV-211:
A letter to CDC Director Mandy Cohen, MD, MPH signed by hundreds of public and occupational health experts noted that the proposed change “allows healthcare employers undefined broad discretion in creating and implementing their infection control and prevention plans,” based in part on staffing levels, patient populations, and a distinction between “pandemic-phase” and “seasonal” pathogens.12 The public response has been “We don’t stop hand washing because norovirus cases are down. We don’t stop wearing gloves because HIV cases are down.”13
In a review of studies comparing N95 respirators to surgical masks, the HICPAC work group concluded that there is “no difference between N95’s and surgical masks” in protecting against viral respiratory infections. The letter to Cohen stated that the review ignored applicable data and studies, study flaws like improper mask use, and did not meet National Institute for Occupational Safety and Health (NIOSH) test standards that are “based on sound science and research.”
Despite new language defining “air” and “touch” transmission, the letter said the proposals ignored aerosol transmission of Covid and “continue to recommend use of surgical/medical masks, which do not provide respiratory protection against infectious aerosols.” Ventilation was not addressed, and the use of airborne infection isolation rooms was limited.
Public commenters reported COVID infections at healthcare facilities after medical professionals refused to wear N95 masks during treatment, and superior wildfire smoke protection from N95 masks over surgical and cloth masks that was easily detected by users: “These things do not make sense, do not protect people, not for fires, not for COVID-19 — both aerosols.”14
Footnotes
- Michael Fox, “Three years into the pandemic, mask usage varies from country to country,” The World, March 7, 2023 ↩︎
- John Yoon and Hikari Hida,”Asia Is Loosening Rules on Masks. Here’s Why People Still Wear Them.” The New York Times, Feb. 2, 2023 ↩︎
- Michael Fox, “Three years into the pandemic, mask usage varies from country to country,” The World, March 7, 2023 ↩︎
- “What were the historical reasons for the resistance to recognizing airborne transmission during the COVID-19 pandemic?” Indoor Air, 21 August 2022 ↩︎
- Neil Vigdor, Jonathan Weisman and Maggie Haberman, “Emulating Trump, Ramaswamy Shows a Penchant for Dispensing With the Facts,” The New York Times, Aug. 30, 2023 ↩︎
- “Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic,” CDC, Updated May 8, 2023 ↩︎
- Michael Lin, MD, MPH and Sharon Wright, MD, MPH, “Isolation Precautions Guideline Workgroup,” HICPAC, June 8, 2023 ↩︎
- Sophie Putka, “CDC Advisory Group Under Fire for Proposed Infection Control Guidelines,” MedPage Today, August 25, 2023 ↩︎
- Julia Doubleday, “Hospitals are killing patients because they don’t feel like doing infection control,” The Gauntlet, Aug 23, 2023 ↩︎
- Sophie Putka, “CDC Advisory Group Under Fire for Proposed Infection Control Guidelines,” MedPage Today, August 25, 2023 ↩︎
- Michael Lin, MD, MPH and Sharon Wright, MD, MPH, “Isolation Precautions Guideline Workgroup,” HICPAC, June 8, 2023 ↩︎
- Sophie Putka, “CDC Advisory Group Under Fire for Proposed Infection Control Guidelines,” MedPage Today, August 25, 2023 ↩︎
- Julia Doubleday, “Hospitals are killing patients because they don’t feel like doing infection control,” The Gauntlet, Aug 23, 2023 ↩︎
- Sophie Putka, “CDC Advisory Group Under Fire for Proposed Infection Control Guidelines,” MedPage Today, August 25, 2023 ↩︎
Reply
You must be logged in to post a comment.